A new DNA sequencing technology is transforming the world of genetic testing. This advanced technology is called Next-Generation Sequencing or NGS, and allows scientists, analysts, and geneticists to process millions of fragments of DNA simultaneously, as opposed to one sequence at a time.
NGS is used for whole genome sequencing, whole exome sequencing, RNA sequencing, metagenomics, and more. Its accuracy and efficiency allow for far reaching applications, from medical research and personalized medicine, to oncology, forensic testing, non-invasive prenatal testing, transcriptomics, and beyond—with many new applications still being explored.
How is NGS Changing the DNA Testing Industry?
NGS is a more efficient and scalable sequencing method and produces better resolution than the commonly used Sanger sequencing method. Sanger sequencing sequences DNA one fragment at a time, which presents challenges for higher volume testing and high-throughput sequencing. NGS is also typically more cost effective than Sagner sequencing when looking at a significant number of targets and can be beneficial for high volume testing.
One application of this technology allows healthcare providers to rapidly and accurately diagnose antibiotic-resistant infections and blood-borne pathogens, so patients can receive an accurate diagnosis and effective treatment, reducing antibiotic overuse. These developments in sequencing have also been instrumental in identifying rare diseases in newborn babies, allowing medical professionals to diagnose and treat genetic diseases earlier in life.
NGS sequencing is also beneficial for forensic scientists, providing them with more detailed information which can be used for genetic genealogy, STR profiling, and predictive phenotyping. Small amounts of nuclear or mitochondrial DNA, and even degraded samples, can provide enough information to identify individuals.
Due to the amount of data generated by NGS sequencing, it requires additional expertise in bioinformatics. Sagner sequencing is a useful tool for many applications, however, it does not produce the vast amount of data that NGS sequencing offers.
How Do Labs Adopt NGS Technology and Remain CLIA Certified and/or ISO Accredited?
As this new technology greatly advances DNA sequencing, there are still a few gaps created by other areas of the industry that have yet to catch up. These gaps can cause a few common pitfalls to be aware of when earning or maintaining ISO 15189 or ISO 17025 accreditation or a CLIA certification.
External Quality Assessment (EQA) Providers and Proficiency Testing (PT)
Finding PT and EQA programs for NGS is still a challenge because not many laboratories are using the technology yet and the development of these quality programs is outpaced by the advancement of this science.
The use of NGS for infectious diseases is growing at a far faster rate than EQA providers can develop the panels required for PT. This has led to a lack of EQA panels for many assays. In addition to the lack of panels, PT providers have not yet come to a consensus on where to set the bar for acceptable test results. For example, one program may require >=80% nucleotide agreement while another may require only >=70% agreement for a pass score. Other providers’ requirements are even lower.
When it comes to metagenomic next-generation sequencing (mNGS), there is also a lack of commercially available metagenomic infectious disease programs which use mNGS to identify a wide range of pathogens, including bacteria, viruses, fungi, and parasites, in a single test. This method can be used to quickly diagnose infections or co-infections and reduce broad-spectrum antibiotic overuse. Because these tests are still gaining clinical validation, there are only a few commercial programs available.
To meet the PT requirements of CLIA or ISO 15189, consider expanding your search for PT providers outside of CAP and API to international providers. Alternatively, if you’re unable to find suitable PT programs, consider collaborating with peer laboratories to conduct interlaboratory comparison (ILC), as ISO 15189 allows for ILC in the absence of competent PT providers.
Validation
Ideally, when validating a test, it’s best to use real clinical specimens as opposed to mock specimens. While resources exist for germline and somatic assays, unfortunately, there is a lack of infectious disease positive residual clinical material to validate the scope of NGS test method, which often necessitates the creation and use of mock samples. Mock samples can be obtained commercially or made “in-house” using reference materials, however, this solution does not address the matrix validation for clinically relevant specimen types. ISO 15189 and CLIA require each test to be validated in the specific matrix it will be used on.
In addition, the bioinformatics pipeline must be validated prior to testing patient samples and any time an update is made to the pipeline. This includes thorough documentation of the update, as well as all validation paperwork. As reference materials are updated, so too should the bioinformatics pipeline in order to reflect the update. It’s important that these changes are documented, and a validation is performed so that it is clear which version of the reference genome was used for each software version, and if there was any inconsistencies or gaps in analysis as the software evolves.
When validating the NGS test method, it’s important to develop a validation plan that covers all aspects of NGS including the bioinformatics pipeline and databases. When creating a validation plan, review peer-reviewed papers on verification and validation of NGS and consult with colleagues, peer laboratories, and other clinical testing experts. If possible, attend industry conferences to learn how other laboratories are validating this method and perhaps share clinical samples to support validation. Organizations including APHL, ASM, WHO, CDC are also reliable resources and offer references and webinars on the subject.
Quality Control (QC) Metrics
Quality control in an NGS lab can look much different than traditional approaches used in most clinical testing laboratories. With traditional clinical diagnostic tests, positive and negative controls are tested and cover all phases of diagnostic testing. This approach provides quality measures at the start and end of the workflow but may not provide sufficient information to determine the success of individual samples or the cause of failures due to complexity of NGS assays.
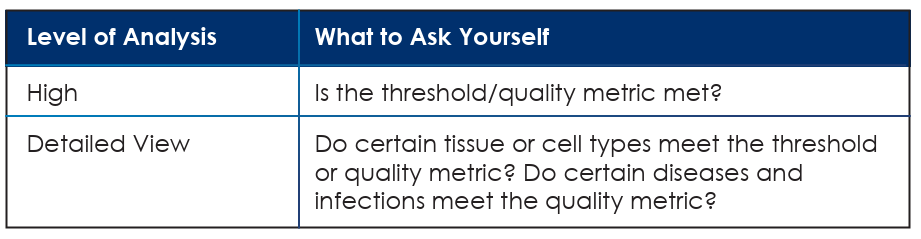
Metrics for NGS testing should track and trend over the entire workflow from sample receipt to report (e.g., extraction, library prep, hybrid capture, sequencing and data analysis), by analyzing metrics such as extraction yields, NTC contamination, read depth, alignment, read length, and quality score, and then analyzing those results at a variety of levels.
Automation
Although automation is not required by CLIA or ISO 15189, the NGS test method typically benefits from automated liquid handling. It’s physically demanding for laboratory staff to pipette NGS workflows with any appreciable volume, therefore automation is imperative. In addition, automated liquid handling is less error-prone than human manipulation of high throughput samples and reduces pipetting errors.
Automation has the added benefit of freeing up staff members’ time to invest in process improvements (i.e., operational excellence) or to complete paperwork for compliance (e.g., NCRs, CAPAs, continuing education, etc.).
NGS is advancing the clinical testing industry and greatly increasing the capabilities of clinical laboratories. Although the requirements of ISO 15189 and CLIA may seem limiting, these requirements provide parameters to successfully utilize this technology to its fullest potential while improving patient outcomes.
For more information about clinical laboratory accreditation, visit A2LA.org/accreditation/clinical-testing.

